#10 Spinal tap problems (lumbar punctures & sometimes epidurals, csf leak)
One for a specific situation
Something to know if offered a spinal tap as an explorative option for a condition, is there can be severe outcomes potentially leaving someone practically immobilised with intense headaches when upright.
With epidurals during labour this is less common as the dura isn’t supposed to be punctured. but it still happens to ~1% of people.
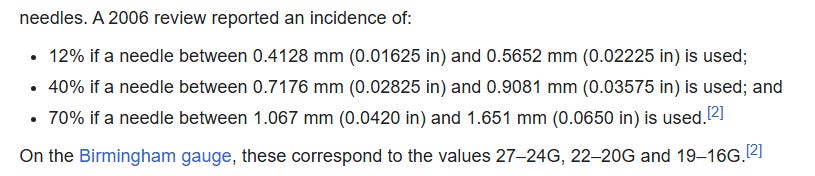
A high incidence of post dural puncture headache occurs, worse with bigger needles. Spinal fluid leak from the puncture site exceeds rate of production, lowering pressure in the brain. After a delay an intense head pain appears from the low intracranial hypotension.
Apparently the dura heals in ~2/3 of people by a couple weeks with minimal movement, with symptoms resolving. But for some people this becomes a chronic condition, barely able or not able to stay upright.
If fortunate a blood patch is given in good time, the persons blood is injected at the dura tear until they feel pain with pressure. The person lays in the same position for a while letting it fully clot which patches the tear and initiates healing.
In very rare cases inflammation in the subarachnoid space or nerve compression can happen because of blood patches, causing neurological problems. Some people notice rebound pressure initially which there are medications for e.g Acetazolamide.
Usually though 1 of these blood patches gives recovery in ~75% of people within symptoms lowering fast if its effective. with maximum chance for effect if they have appropriate rest in the early hours and first week especially.
The clot forms well by 7 - 13 hours, and likely by 7 days the leak is being repaired well with collagen formed.
https://www.anesth-pain-med.org/upload/pdf/apm-21113.pdf
Epidural plug theory supposes that the formation of a gelatinous plug, induced by interactions between the injected blood and procoagulant components in leaking CSF, seals off the dural tear until the natural healing process restores the integrity of the torn dura.
MRI studies have found that epidural blood adheres to the thecal sac, resulting in clot formation for 18–24 h [7]. At 7–13 h, there is clot resolution, leaving a thick layer of mature clot over the dorsal part of the thecal sac. Animal studies have demonstrated that 7 days after the administration of an EBP, there is widespread fibroblastic activity and collagen formation [9]. That is consistent with the time course of PDPH observed in clinical practice but fails to account for the rapid and often immediate relief upon receiving an EBP.
But,
there’s a % of people who still have the problem after a blood patch, especially when non targeted. the process of getting one can be long. and looking around i’ve seen people being refused a patch even though they’re still having intense ongoing positional head pain for months.
There’s 1 herb / mechanism that might create some good relief shown in an interesting case report,
https://pmc.ncbi.nlm.nih.gov/articles/PMC9236673/#sec2
Here a teenager had head pain when standing or playing the saxophone, which stopped when laying down. It started a year earlier, and she showed leakage of CSF by the incomplete floating dural sac sign on an MRI.
She was treated with 7.5g daily of a herb called Goreisan (a mix of herbs) which was split between 3 doses,
Her headaches improved slightly by 1 month, by 2 months her headaches improved drastically with the score reduced from 8/10 to 2/10, and by month 3 she only had 2 occurrences a month.
After that she was free from head pain for the rest of the followup
The orthostatic headache first appeared only when she practiced saxophone with Valsalva maneuver. From the age of 14 years, it began to present for a while after she stood up without playing the saxophone. It gradually aggravated from the age of 15 years, and daily activity was disturbed. Her orthostatic headache was bilateral, with a numerical rating scale (NRS) of 8/10 and no pulsing symptoms. Every day, she had a headache. No nausea, photophobia, or phonophobia was present.
The headache did not develop while lying down or sitting, but only after standing for a few minutes. She claimed that her headache got worse as she played the saxophone while standing and sitting
The incomplete floating dural sac sign was shown
She wanted to continue playing saxophone and did not want to be admitted. Therefore, we prescribed 7.5 g of Japanese herbal Kampo medicine Goreisan to treat suidoku status (fluid disturbance such as edema, dehydration, and dislocation) [5,6,8] in three divided doses. The headache severity slightly improved over one month.
After one month, her headache was relieved as her NRS score was 2/10, and it occurred two times per month from the next month. Then, her headache has never recurred for one year, and she can still now play the saxophone, intaking Goreisan 7.5 g/day in three divided doses. Her family doctor will reduce Goreisan to 5.0 g/day in two divided doses, 2.5 g/day as a single dose, and 2.5 g as needed over some years. The follow-up MRI will be performed in the future.
And here 18 people with cerebrospinal fluid hypovolemia were treated with Goreisan. (those that had a blood patch but still had remaining symptoms, nausea vomiting and dizziness).
with the majority 12/18 showing 50% or more relief. They used 7.5g divided into three doses
(no apparent improvement was defined as < 50%, meaning the remaining 6 people still could have improved with up to 49% relief too)
https://www.jstage.jst.go.jp/article/jnkm/1/1/1_03/_article/-char/en
A study investigated the effect of Goreisan, a diuretic Kampo medicine, on 18 patients diagnosed with CSF hypovolemia who continued to experience nausea, vomiting, and dizziness after blood patch treatment. The dosage was 7.5 g/day divided into three doses.
Seven cases (38.9%) showed good recovery (relief ≥ 75%), 5 cases (27.8%) showed moderate recovery (relief ≥ 50%), and 6 cases (33.3%) showed no apparent improvement (relief < 50%) by the administration of goreisan
Since the 1970s, alternative absorption pathways, such as lymphatic absorption via spinal nerve roots, have gained attention.In CSF hypovolemia cases, imaging studies suggest a CSF absorption route via spinal nerve root meninges exists, especially in pathological states. CSF does not circulate but diffuses and mixes, and arachnoid granulations near the sagittal sinus are unlikely to be the main absorption site.
The improvement of nausea, vomiting, and dizziness after Goreisan administration suggests its diuretic effect may contribute to improving CSF dynamics, offering new insights into the disease mechanism.
The aquaporins (e.g AQP4) are highly involved in water transport in and out of cells. Its role in edema is context dependant, it can help water exit / prevent extra buildup from high extracellular water, but can also increase entry.
There seems to be some benefit to inhibiting it for people with CSF leak, unless this wasn’t the main mechanism.
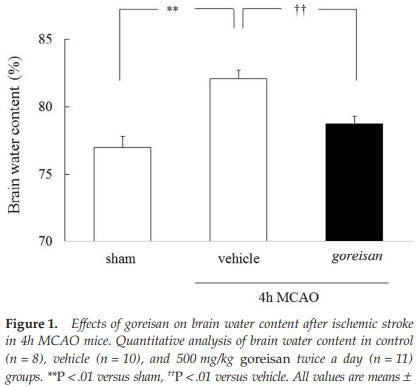
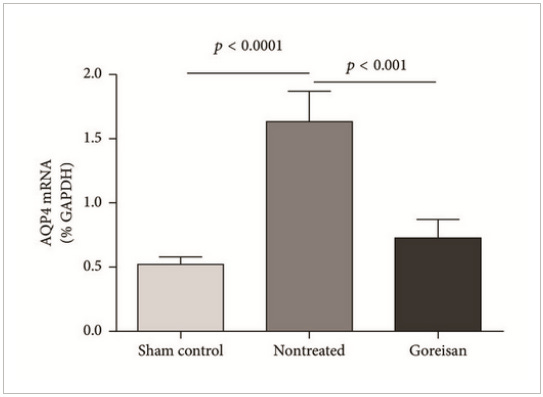
Goreisan has been shown to reduce AQP4 expression in brain pathology, and lower brain edema,
here in ischemic brain edema, it reduced the increase in brain water / swelling https://pubmed.ncbi.nlm.nih.gov/29153303/
and when used for a short time here, with AQP4 inhibition
https://onlinelibrary.wiley.com/doi/10.1155/2017/3209219
Goreisan significantly suppressed AQP4 protein level in the chronic phase but did not have a significant effect in the acute or subacute phases.
Goreisan has been suggested to prevent the water trafficking function of AQP4;
Goreisan treatment did not change AQP4 levels during the acute phase, indicating that Goreisan does not have a direct effect on AQP4 gene transcription itself. Indeed, administration of Mn2+ and Mg2+, which are important components of Goreisan, to our animal model of edema produced no suppressive effects on AQP4 mRNA (data not shown). These results collectively suggest that the decreased AQP4 mRNA and protein levels are secondary events among various other changes to mRNAs and proteins that are induced by Goreisan treatment.
Although being a secondary effect, AQP4 levels were influenced by Goreisan and correlated with an improved survival rate. We, therefore, propose one of the effects of Goreisan is inhibition of AQP4.
The chronic phase is followed by the resolution phase when there is a net movement of water from brain to blood. In this phase, a reduced AQP4 level is a disadvantage rather than an advantage in improvement of edema. The precise time of onset of the resolution phase is debatable, but prominent resolution can be seen around day 7 after the onset of edema.
Western blotting revealed that levels of AQP4 protein were significantly decreased in the Goreisan group compared with the nontreated group in the lesion side 72 h postoperatively, but not at 12 or 36 h.
But these are showing short term dynamics,
in the case report it took a month or 2 to start gaining the profound result. which makes me wonder if it gave a progressive foundational fix over time.
Whatever the mechanism, whether its through changing fluid dynamics or through accelerating repair of the dura or something else, it seems Goreisan could have a great effect here over time.
Its a mix of 5 powdered herb extracts :
4 parts Alisma Tuber (tuber of Alisma orientale Juzepczuk),
3 parts Polyporus Sclerotium (sclerotium of Polyporus umbellatus Fries),
3 parts Poria Sclerotium (sclerotium of Poria cocos Wolf),
3 parts Atractylodes lancea Rhizome (rhizome of Atractylodes lanceae De Candolle),
1.5 part Cinnamon Bark (Cinnamomum cassia Blume)
To try to replicate results obviously the Goreisan mixture is best, the herbs might be synergistic.
But if someone is in a location where they don’t have access to this and cant get all of them, the Atractylodis Lanceae Rhizoma could be a main part of the effect. Thats unknowable without isolated tests though.
A related species Atractylodis macrocephalae has effects on AQP2 at least https://pmc.ncbi.nlm.nih.gov/articles/PMC3522508/#abstract1. And they both have effects on increasing wound healing. cinnamon is a small part of the formulation, and its 1 i’ve seen some toxicity concerns with. But obviously just using 1 isn’t replicating the studies.
If trying its probably a good idea to make sure each 1 is decently safe and i'd start small initially just to be on the safer side, its got a long history of use in japan and a good safety profile by animal studies https://www.jstage.jst.go.jp/article/tmh/42/3/42_2014-04/_pdf/-char/en
Personally i'd skip the cinnamon if i was trying to put it together without access to the herb. but thats me, and it wouldn’t be replicating study fully.
Atractylodes Lancea (also known is cang zhu , which refers to a couple atractylodes plants that are very similar)
atractylodes Macrocephala (bai zhu) also has some similar compounds, possibly could fit as a replacement. but it has a lower % of compounds than Atractylodes lancea so its less potent. theres some differences in compounds so it could make a difference from the actual type they used.
Both have atractylone, cang zhu has more though (~1.32% of the dry weight vs ~0.2% - 1%) plus Atractylodin at a few %.
Atractylodes lancea has yellow or dark orange spots over it if good quality.
As far as i can tell these are both it
Where the other bai zhu type is more pale throughout
Cant ingest it as chunks of rhizome so it needs powdering. or a less potent way if can’t get the powder is boiling it as a tea + microwaving for 5 mins to get more of the oils out. It’s used in china a lot but I always allergy test small amounts of new things.
There’s trials using a combination of medications, neostigmine and atropine for acute relief, with some side effects. https://pubmed.ncbi.nlm.nih.gov/30169405/