Generally, broadly increasing serotonergic activity creates anxiety, fear, withdrawal & fatigue.
It’s high in chronic fatigue syndrome and autism, and research in recent years highlights the “Low serotonin” narrative for depression as the mainstream view for decades has been false.
Serotonin is not lower in people with depression, stress increases serotonin, and some areas of the brain show high serotonin in people who committed suicide (and in a notably violent way).
Some papers highlighting why raising serotonin is probably not the best idea with mood disorders:
Serotonin not lower in people with depression
https://www.sciencedaily.com/releases/2022/07/220720080145.htm
Co-author Dr Mark Horowitz, a training psychiatrist and Clinical Research Fellow in Psychiatry at UCL and NELFT, said: "I had been taught that depression was caused by low serotonin in my psychiatry training and had even taught this to students in my own lectures. Being involved in this research was eye-opening and feels like everything I thought I knew has been flipped upside down.
Professor Moncrieff added: "Thousands of people suffer from side effects of antidepressants, including the severe withdrawal effects that can occur when people try to stop them, yet prescription rates continue to rise. We believe this situation has been driven partly by the false belief that depression is due to a chemical imbalance. It is high time to inform the public that this belief is not grounded in science."
Our comprehensive review of the major strands of research on serotonin shows there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity. Most studies found no evidence of reduced serotonin activity in people with depression compared to people without,
Weak evidence from some studies of serotonin 5-HT1A receptors and levels of SERT points towards a possible association between increased serotonin activity and depression. However, these results are likely to be influenced by prior use of antidepressants and its effects on the serotonin system
Research that compared levels of serotonin and its breakdown products in the blood or brain fluids did not find a difference between people diagnosed with depression and healthy control (comparison) participants. Very large studies involving tens of thousands of patients looked at gene variation, including the gene for the serotonin transporter. They found no difference in these genes between people with depression and healthy controls.
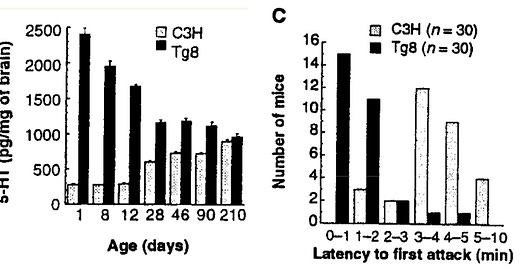
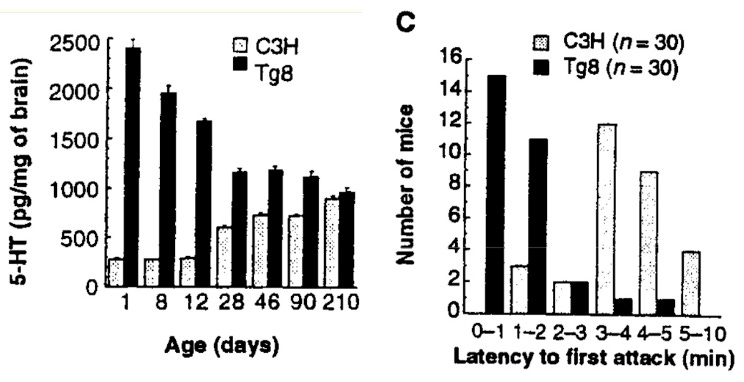
High serotonin signalling can also create aggression, which with the other effects is likely a fear based complexity-rejecting aggression in high stress (shown in rats through inhibiting the MAO-A enzyme causing a big increase in serotonin. the rats became on edge, attacking other rats fast https://pmc.ncbi.nlm.nih.gov/articles/PMC2844866/
Pup behavioral alterations, including trembling, difficulty in righting, and fearfulness were reversed by the serotonin synthesis inhibitor parachlorophenylalanine
similar effects show in extreme autism, which comes with higher serotonin levels https://pmc.ncbi.nlm.nih.gov/articles/PMC6215718/).
Our subsequent analyses disclosed that the behavioral repertoire of MAO A KO mice reproduced all major core deficits observed in autism-spectrum disorder (ASD), including social deficits (indicated by lower social approaches towards either freely moving or caged counterparts) and communication impairments.
The finding of autistic-like phenotypes in MAO A KO mice was strikingly confirmed by later clinical findings. Indeed, in 2014, the employment of targeted high-throughput sequencing methodologies in a broad sample of individuals with intellectual disability enabled the identification of a new case of MAOA deficiency in a 7-year old boy diagnosed with ASD, attention deficit and self-injurious behavior (Piton et al., 2014). The corresponding mutation was a substitution of cysteine 266 to a phenylalanine, which caused a drastic reduction in catalytic activity, estimated to be 10–40 times lower than normal levels
Here’s a direct intervention study showing the effects in mammals,
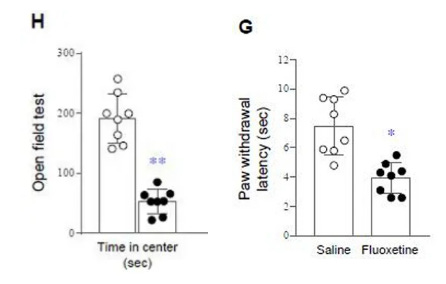
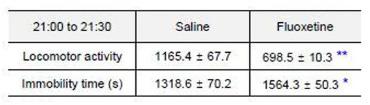
a SSRI induced fatigue, anxiety and lower tolerance to pain through serotonin
https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04808-x
Time spent in the center of the area (a measure of how much anxiety they have) dropped much lower with those given the SSRI (black dots) showing they were put in fear by the serotonergic signalling
And decreased their ability to withstand pain by half (right)
Their overall activity / movement time also decreased a lot (fatigue)
Serotonin increase in the brain is generally connected to a state of helplessness,
when researchers gave a mild uncontrollable stress to rats, they developed a state of helplessness and tried to escape less. When they severely depleted serotonin in the brains, their will to try was restored https://pubmed.ncbi.nlm.nih.gov/2945212/
The severe depletion of 5-HT in various brain regions was highly correlated with a dramatic improvement in the shock escape scores.
These experiments implicate the serotonergic system as a possible mediator of the "learned helplessness" phenomenon.
Inescapable stress increases serotonin in the DR region of the brain, and the TRPH2 enzyme (creates serotonin in the brain) is found high in this region in people who committed suicide.
Stress increases TRPH2
Inescapable tail shock was sufficient to increase tph2 mRNA expression 4 h and 28 h later, selectively in the dorsomedial DR (caudal aspect of the dorsal DR, cDRD; an area just rostral to the caudal DR, DRC) and increased Tph2 protein expression in the DRD (rostral and caudal aspects of the dorsal DR combined) 24 h later.
https://www.researchgate.net/publication/322542359Expression of TPH2, the rate-limiting enzyme for brain serotonin synthesis, is elevated in the dorsal raphe nucleus (DR) of depressed suicide victims.
One hypothesis is that this increase in TPH2 expression is stress-induced
Risk of suicide increases 5x during initial month of raising serotonin with SSRIs
https://pubmed.ncbi.nlm.nih.gov/16648321/
(fitting with these taking a while to show effect (if they do show improvement, not a great effectiveness rate, if they don’t make things worse or drive someone to suicide), indicating its a secondary countering response to the serotonin increase, or an alternative increase like acting on BDNF or neurosteroids in the brain, or fixing the early increase in REM sleep with depression which interferes with deep sleep, and serotonin being the harm)
During the first month of therapy, SSRI antidepressants were associated with a nearly fivefold higher risk of completed suicide than other antidepressants
Ironically, a mainstream approach to treating depression has been through trying to raise a neurotransmitter that generally increases negative emotion. And as a basic standard / not a final resort.
Psychosis
Another interesting connection here, a lot of focus on the effectiveness of anti-psychotics is on dopamine blocking. Things get complicated here with serotonin-dopamine interactions, pre vs post synaptic effects, specific receptors etc.
But something anti-psychotics have in common is they’re basically all inverse agonists at the 5ht2a & or 5ht2c receptor (5ht2a receptor can induce hallucinations when activated in a certain way), inverse agonists lower the amount of signalling. https://pubmed.ncbi.nlm.nih.gov/10991983/.
People with psychosis / schizophrenia already have low dopamine signalling in the striatum, apparently selectively antagonising d2 in the right regions can help with positive symptoms (? im still not convinced) but not the lacking dopamine signalling, apathy depression low reward etc. BUT blocking the 5ht2a serotonin receptor eases the positive symptoms https://www.nature.com/articles/s41380-024-02531-7 and they discovered even haloperidol which is best known for d2 antagonism also has effect at blocking serotonin signalling (acting as full antagonist at g protein pathways
We tested the antipsychotics for their effect on the 5-HT (EC80)-mediated activation of the different G protein pathways and on the recruitment of β-arrestins. As was observed in the agonist mode, the inverse agonist activity of risperidone, clozapine, olanzapine and haloperidol could be seen at Gαq, Gα11 and Gα14 as reflected by the fact that the compounds not only fully antagonized the 5-HT-promoted BRET response but also promoted a BRET reduction below basal activity (Fig. 4a–c and Supplementary Table 4b).
For Gα15, Gαz, Gαi1, GαoB and the β-arrestins, the four compounds behave as full antagonists and no inverse agonist activity could be detected Previous studies have implicated Gαi1 signaling through 5-HT2AR activation in the mechanism of action of hallucinogenic drugs, and a supersensitive coupling of 5-HT2AR to Gαi1 as opposed to Gαq has been identified in the postmortem brain samples of schizophrenia patients.
And this approach is proven in humans, proof that dopamine blockade is not needed to ease positive symptoms and that dopamine defects associate with psychosis (people with parkinsons get it). giving them pimavanserin which is an inverse agonist or antagonist at 5ht2a helps with the hallucinations / delusions
Pimavanserin, which has been reported to be an inverse agonist at the 5-HT2AR/Gαi1 pathway has been approved for Parkinson’s disease-associated hallucinations and delusions.
you can induce hallucinations in mammals by activating 5ht2a in a certain way. elevating serotonin can cause extremes of negative emotion including fatigue. i wrote a bit about these here https://cs3001.substack.com/p/serotonin-an-unhappy-neurotransmitter
and antagonising 5ht2a when haloperidol is given helps lower the depression caused by it https://pubmed.ncbi.nlm.nih.gov/16794561/
Organic molecules in the body can obviously serve a helpful purpose at the right times, there are likely areas where a certain amount of serotonin signalling is useful. but by these serotonin is generally very undesirable for mood, and i would want to avoid increased levels.
If someone is in a state of hypothyroidism, this is key to fix for overall baseline mood, as depression comes with a high rate of hypothyroidism. (can be indicated by a low core temperature < 37 degrees celsius measured under the tongue with a thermometer. a TSH measure on blood panel isnt enough to tell alone and might be set too high, and a decent number of people have issues converting t4 to the active t3 hormone.
when testing its better to wait a bit after waking, as high adrenaline overnight could prevent some heat loss through constricting blood vessels
more on thyroid hormone here: https://raypeat2.com/articles/articles/thyroid-insanities.shtml
When measuring T3, the most important thyroid hormone, 90% of depressed patients were low in this group of people, even though only 19% of them would have shown up as hypothyroid by looking for raised TSH alone compared to non depressed controls with higher T3.
https://pmc.ncbi.nlm.nih.gov/articles/PMC2958345/
In this study, 32 unmedicated patients of unipolar depression were included and blood samples were analysed for T3, T4 and TSH. These were compared with age and sex matched controls. Subnormal T3 and T4 levels in 90.6% and 9.3% respectively and an increase of TSH levels in 18.7% of the total patients was observed in this study.
Such high rates aren’t a common finding everywhere, but they also showed the degree of depression correlated with the drop in T3.
Going to write up a separate post highlighting why there’s such a big connection & its effects
While fixing the baseline, Aspirin (if tolerated without allergy, and if tapered off of SSRIs as there’s increased bleeding risk when mixing, and using dispersible form to lower risk of harm to the gut, avoiding enteric coated forms), Coconut oil / coconut flakes, 200mg vitamin C, and avoiding pufa & fish oil if taking, are some things that might have beneficial effects on mood shorter term.
Estrogenic signalling can also act as serotonergic signalling if high, as estrogen acts to increase serotonin through the TPH2 enzyme, and can upregulate the 5ht2a receptor. https://pmc.ncbi.nlm.nih.gov/articles/PMC5825233/
High estrogen relative to the hormone progesterone is associated with high stress, with more activity in the amygdala.
Progesterone drops a lot after menopause, and some women find restoring their progesterone helpful to fix insomnia & stress post menopause. And in postnatal depression too, after high progesterone production from the placenta goes away. (using bioidentical hormone, not the synthetic progestins). a subset of women might not notice much of a helpful response, which might be related to either poor or excess conversion to the neurosteroids used to treat postnatal depression.
This study is insightful here, measuring variability in mood over weeks in women with depression, showing 90% of them had estrogen levels spiking over normal levels, and lack of progesterone reaching good levels https://pmc.ncbi.nlm.nih.gov/articles/PMC7075107/#s8
Polyunsaturated fats in diet (e.g from seed oils) have estrogenic signalling (more on this at https://haidut.me/?p=2360 , great blog) so have the potential to increase stress.
Fish oil has some toxic breakdown products, whether its oxidized outside the body or inside. when trying fish oil with hypothyroidism my core temperature dropped noticeably, with worse mood.
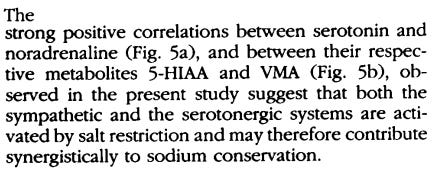
A diet too low in salt can raise serotonin a lot, at least shown peripherally https://pubmed.ncbi.nlm.nih.gov/7510737/
The serotonin transporter is dependant on sodium.
So people restricting salt might want to consider this if they’re noticing higher stress.
Both adrenaline and serotonin can contribute to stress. Salt can also help lower adrenaline, and the effects of salt on heart disease is exaggerated, with a bigger area for safety than might be commonly communicated. over-restricting is also associated with harms.
https://raypeat.com/articles/articles/salt.shtml
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)30467-6/abstract?rss=yes
Sodium restricted diets aside, people with hypothyroidism (& high rates of mood disorders with this) waste a lot of sodium, and can notice high adrenaline routinely (especially at night).
In squirrels the MAO enzyme decreases and serotonin elevates when going into hibernation (and not as much during). https://www.sciencedirect.com/science/article/abs/pii/0091305781903609
So its functioning to prepare them for hibernation, getting mammals to reject / withdraw from the world long term into a shut down state in a hole. sounds like depression.
Hit follow on my profile, or get updates for new posts, no cost:
Paste the link to someone in a related discussion if you found this insightful



Nice article! Any studies with sun exposure and serotonin levels?
Thanks for your work!